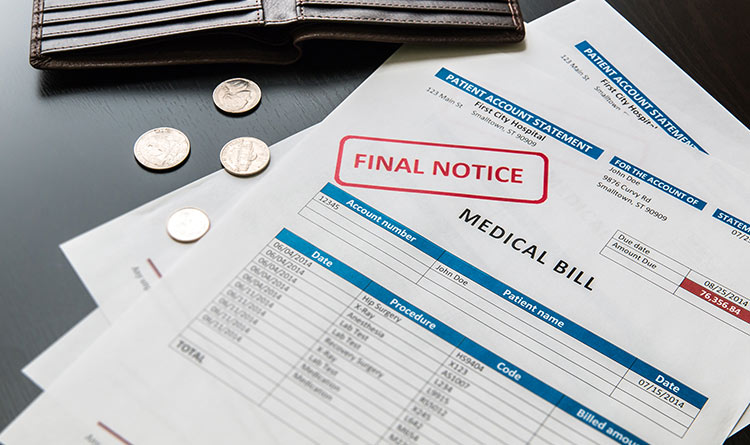
While there aren’t comprehensive statistics on medical billing errors, Boston-based healthcare advocacy group Access Project estimates that up to 80% of medical bills include errors. In most cases, a lack of proper training, understaffing, lack of pre-authorization procedures, and using out-of-date medical codes are the main contributors to medical billing errors.
Additionally, many government policies such as Medicaid and Medicare are zero-tolerance. As a result, healthcare providers cannot afford any mistakes when submitting claims or miss out on reimbursement opportunities. Fortunately, you can adopt these practices to prevent the costly consequences of medical billing errors – read on to find out more!
Stay Up-to-Date on the Latest Medical Codes
Using the wrong or outdated medical codes play a huge role in delaying the claims submission process. Billing departments in healthcare organizations should stay up-to-date on the latest billing standards and regulations to ensure a first-pass claim submission. One way to do this is to have your organization representatives attend seminars by the regulatory and authoritative bodies to get the latest up-to-date information. Additionally, your staff should always have access to the latest coding manual to refer to for the appropriate billing processes.
Outsource a Medical Billing Company
Sometimes, outsourcing for external help might be the smartest financial decision you can make. While your staff and organization focus on providing the best quality healthcare to your clients and patients, a third-party medical billing company like KR Billing Solutions can help significantly in expediting and streamlining your billing operations and processes. You get to take advantage of the latest automation software, programs, and claims scrubbing services that can maximize your organization’s cash flow and revenue. Additionally, you can leave the job of staying updated on the ever-changing rulebook of medical codes to the billing company.
Double Check the Patient’s Particulars and Eligibility
While it might sound silly that a trivial error such as missing out a digit of the policy number or forgetting a letter in the patient’s name can be grounds for a claim denial, this reality remains that these often-overlooked details are the cause of many rejections. Additionally, the patient’s eligibility could change based on their coverage terms with the insurance company. Therefore, as a rule of thumb, healthcare providers should have the practice of verifying the patient’s information before performing any form of healthcare service and before submitting the claim. These routine practices could play a critical role in maximizing your revenue cycle and reducing the number of errors in your medical billing processes.
Consider Automating Your Billing Processes
Integrating technology into your billing processes can be a costly investment for any company. However, this would be beneficial in reducing trivial and often-overlooked human errors in the long term. These medical billing software programs are designed to check and match the data against any electronic health record stored in the system, preventing common medical coding mistakes and reducing the chances of claims denial. Additionally, this could go a long way in helping your staff focus and channel their efforts to provide the best quality healthcare service to your patients.
Maximize Your Revenue with KR Billing Solutions
With many years of prior experience in the medical billing industry, KR Billing Solutions specializes in providing various billing services, including clearinghouse tracking, patient billing, claim scrubbing and submission, and more. We are delighted to work with all primary healthcare providers and explore maximizing their cash flow and revenue cycle. At KR Billing Solutions, we are determined to provide contemporary and effective solutions to optimize your medical billing processes.
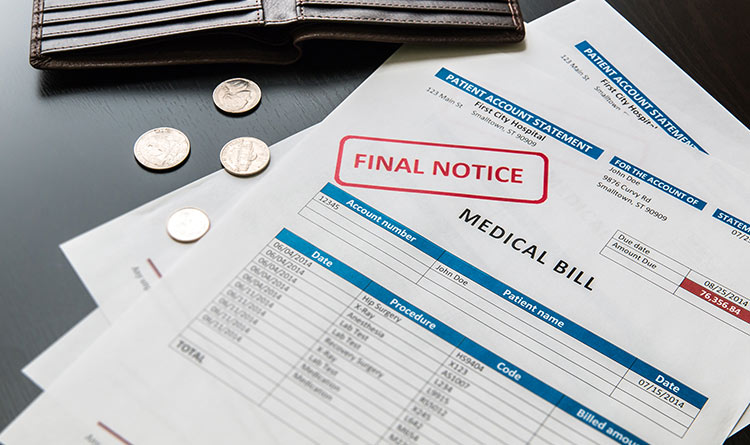
While there aren’t comprehensive statistics on medical billing errors, Boston-based healthcare advocacy group Access Project estimates that up to 80% of medical bills include errors. In most cases, a lack of proper training, understaffing, lack of pre-authorization procedures, and using out-of-date medical codes are the main contributors to medical billing errors.
Additionally, many government policies such as Medicaid and Medicare are zero-tolerance. As a result, healthcare providers cannot afford any mistakes when submitting claims or miss out on reimbursement opportunities. Fortunately, you can adopt these practices to prevent the costly consequences of medical billing errors – read on to find out more!
Stay Up-to-Date on the Latest Medical Codes
Using the wrong or outdated medical codes play a huge role in delaying the claims submission process. Billing departments in healthcare organizations should stay up-to-date on the latest billing standards and regulations to ensure a first-pass claim submission. One way to do this is to have your organization representatives attend seminars by the regulatory and authoritative bodies to get the latest up-to-date information. Additionally, your staff should always have access to the latest coding manual to refer to for the appropriate billing processes.
Outsource a Medical Billing Company
Sometimes, outsourcing for external help might be the smartest financial decision you can make. While your staff and organization focus on providing the best quality healthcare to your clients and patients, a third-party medical billing company like KR Billing Solutions can help significantly in expediting and streamlining your billing operations and processes. You get to take advantage of the latest automation software, programs, and claims scrubbing services that can maximize your organization’s cash flow and revenue. Additionally, you can leave the job of staying updated on the ever-changing rulebook of medical codes to the billing company.
Double Check the Patient’s Particulars and Eligibility
While it might sound silly that a trivial error such as missing out a digit of the policy number or forgetting a letter in the patient’s name can be grounds for a claim denial, this reality remains that these often-overlooked details are the cause of many rejections. Additionally, the patient’s eligibility could change based on their coverage terms with the insurance company. Therefore, as a rule of thumb, healthcare providers should have the practice of verifying the patient’s information before performing any form of healthcare service and before submitting the claim. These routine practices could play a critical role in maximizing your revenue cycle and reducing the number of errors in your medical billing processes.
Consider Automating Your Billing Processes
Integrating technology into your billing processes can be a costly investment for any company. However, this would be beneficial in reducing trivial and often-overlooked human errors in the long term. These medical billing software programs are designed to check and match the data against any electronic health record stored in the system, preventing common medical coding mistakes and reducing the chances of claims denial. Additionally, this could go a long way in helping your staff focus and channel their efforts to provide the best quality healthcare service to your patients.
Maximize Your Revenue with KR Billing Solutions
With many years of prior experience in the medical billing industry, KR Billing Solutions specializes in providing various billing services, including clearinghouse tracking, patient billing, claim scrubbing and submission, and more. We are delighted to work with all primary healthcare providers and explore maximizing their cash flow and revenue cycle. At KR Billing Solutions, we are determined to provide contemporary and effective solutions to optimize your medical billing processes.




Recent Comments