- Home
- Our Services
- AR Follow Up
AR Follow Up
AR Follow Up
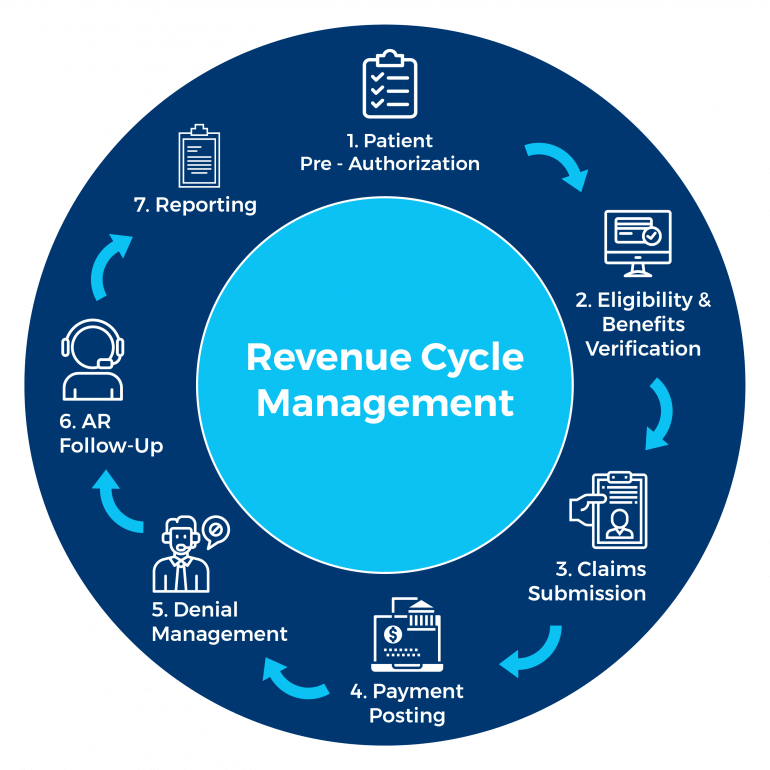
KR Billing Solutions has worked with numerous insurance companies, healthcare providers and is well-versed with their policies and billing process. We have a broad range of expertise in the medical sector and believe in helping healthcare providers maximize their revenue by making the billing and claiming process more efficient. We provide billing services and revenue cycle management for our clients to ensure reliable and quick processing of claims.
About AR Follow Up
Accounts Receivable (AR) refers to the money owed to healthcare providers or medical billing companies for the medical care and services they render to the patient. The invoices which are generated are then sent out to patients and insurance companies for payment.
AR follow-up thus refers to the processes involved such as minimizing AR days, eliminating aged AR, re-filing corrected claims, and identifying denied or unpaid claims. AR follow-ups thus ensure that healthcare providers can continue running their services successfully and smoothly while ensuring the AR or money owed is refunded back as soon as possible.
The AR follow-up team is also responsible for looking after the denied claims and renewing them to get maximum reimbursement from the insurance companies. If specific and constant AR follow-up is not done on the current billings initiated, healthcare providers may be faced with an excessive amount of medical AR that is due for a long period such as 180 days or more.
This would affect the cash flow, revenue, and sustainability of the healthcare providers in providing their healthcare services to patients.
Key Features of AR Follow Up
The primary responsibility of AR follow-up is to recover overdue payer or patient payments. There are several phases and features involved in the AR follow-up process.
Initial Evaluation
This stage involves identifying and analyzing claims listed on the AR aging report. The AR follow-up team then reviews the healthcare provider’s adjustment policy to identify the more urgent and earlier claims which have to be adjusted. Once timely filings of the claim are conducted, the provider may choose to identify additional claims
Analysis and Prioritizing
Experienced medical AR analysts initiate this phase by identifying the various problems and issues for the denied or uncollectible claims. This could also be the case for claims where the healthcare provider has not been paid according to its contracted rate with the insurer. The appeal and filing limits of the healthcare providers will be checked and the AR follow-up team ensures that the clean claims are reimbursed as per the contracted timeline.
Collection
The claims identified are re-filed after verifying all the necessary billing information. After completing the posting of payment details for the outstanding claims, patient bills are generated according to the client’s guidelines and followed up with the patients for payment.
Why Choose KR Billing Solutions?
KR Billing Solutions has a highly experienced team of AR specialists that ensure our clients do not face any difficulties in receiving payment for their medical services. We have the resources and software necessary to verify the accuracy and comprehensiveness of the data provided during the billing process. This allows you to focus on your primary responsibility of patient care and treatment while we manage the billing and claims process for you.
If you have any questions about AR follow up, you can call us at (855) 978-6499 or send us an email.
Need Our Help?
Prefer speaking with a human to filling out a form? call corporate office and we will connect you with a team member.
