- Home
- Our Services
- Claim Scrubbing & Submission
Claim Scrubbing & Submission
Claim Scrubbing & Submission
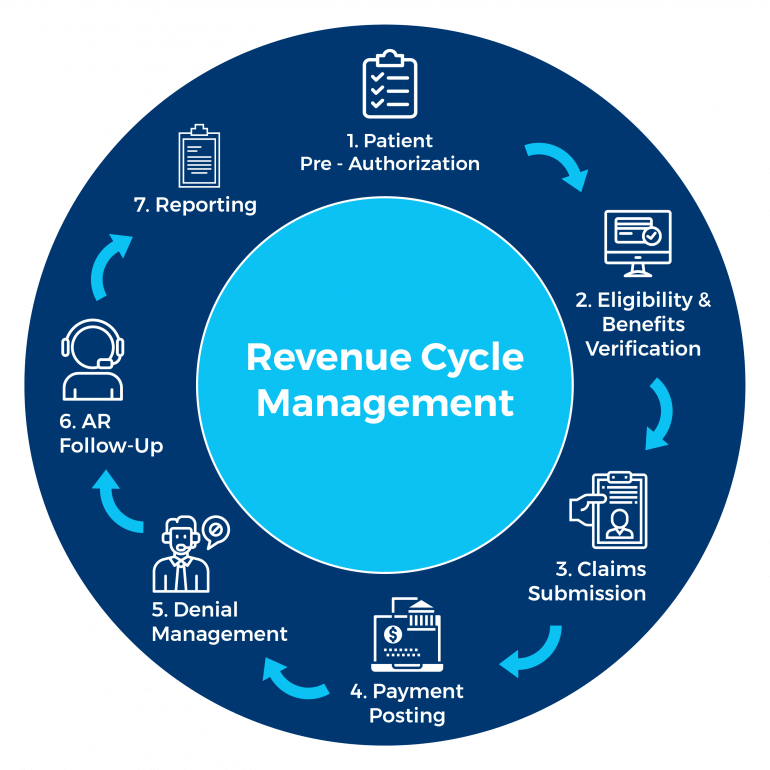
KR Billing Solutions provides various financial services to help with your company’s revenue cycle management and optimize the billing process. Our billing service can help healthcare companies maximize their revenue, account for their transactions while ensuring clients benefit from our wide range of expertise in the medical sector.
About Claim Scrubbing & Submission
Claim scrubbing and submission is an important process of the billing cycle that can determine whether or not medical companies get their reimbursement from the insurer. Claim scrubbing refers to the process of reviewing the claim data to check for any errors and ensuring that all the claim information is complete and correct.
This has to be done before the claim is submitted to payers. Most claim scrubbing processes are automated to save time and manpower costs for the insurance company. Claim scrubbing also involves checking the healthcare provider, patient, and medical treatment information as well as the medical diagnosis, treatment, and modifier codes. These data are reviewed and analyzed and if everything is correct, the claim can then be submitted.
Claims scrubbing also helps to detect common issues which may lead to the claim being rejected such as invalid diagnosis code, invalid member identification, and missing admission date of the patient. Small mistakes and misinformation such as the wrong date of birth or a misspelled name may cause the insurance company to reject the claim and send it back.
Key Features of Claim Scrubbing & Submission
Because claim scrubbing involves verifying and assessing all claim information to be correct before claim submission, claims which have been scrubbed and are submitted afterward have a much higher chance of being accepted, resulting in reimbursement of the claims to the medical provider.
Claim scrubbing also ensures that there are no mistakes made in the medical claim that would lead to the insurance company denying the medical claim. The features and benefits of claim scrubbing are cleaner claims, less work, fewer denials, more cash flow, and faster payment. By submitting an accurate claim the first time, payers can pay the healthcare company on time, thereby increasing the revenue and cash flow of the healthcare company to cover its needs.
Claim scrubbing also makes the entire medical billing process significantly easier as all the information has been verified and assessed. Claim scrubbing also verifies that all CPT codes in a medical claim are accurate. Claim scrubbing is also proven to improve payer and patient relationships.
Why Choose KR Billing Solutions?
When medical claims go through quickly, it can save the insurer, patient, and provider valuable time and money as well as prevent frustration between the parties involved. KR Billing Solutions can increase claim accuracy and improve your business’ cash flow through the submission of clean claims. We can help you optimize your staff time, reduce your claim denials and create better relationships with your payers. This also indirectly supports patient retention in your business and improves your business’ revenue management.
If you have any questions about claim scrubbing and submission, you can call us at (855) 978-6499 or send us an email.
Need Our Help?
Prefer speaking with a human to filling out a form? call corporate office and we will connect you with a team member.
