- Home
- Our Services
- Denial Management & Appeals
Denial Management & Appeals
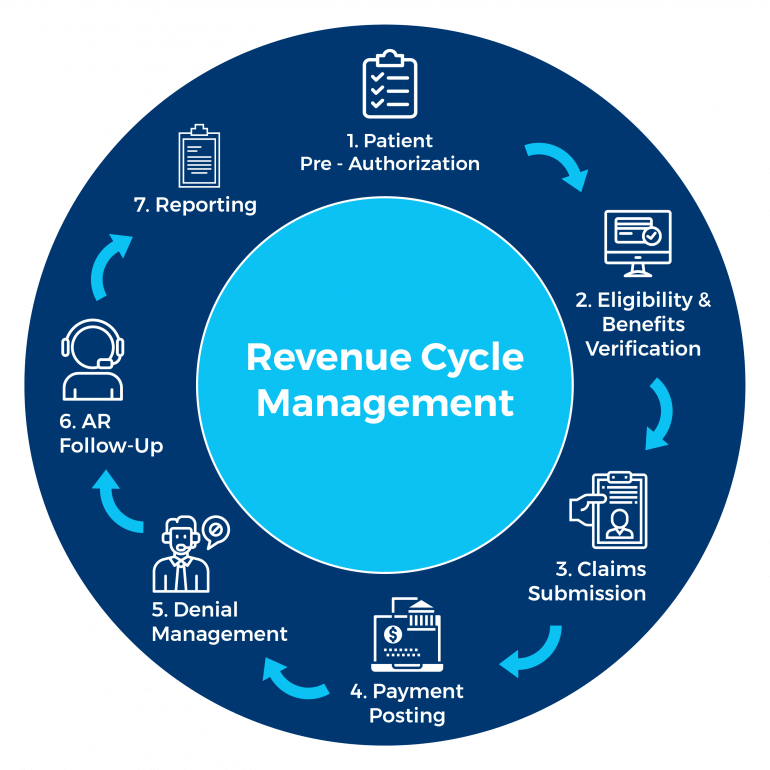
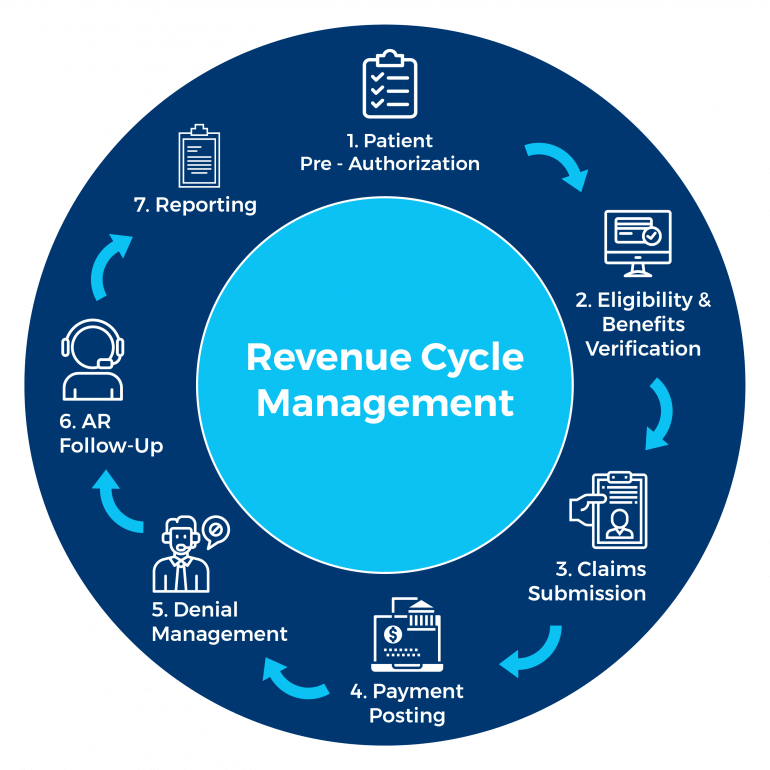
KR Billing Solutions can handle all your billing needs and help you manage your revenue cycles to maximize your revenue and ensure constant cash flow. We have the capacity, software, and team members to handle the high volume of claims and denials and can address any lost revenue during our audits and tracking services.
About Denial Management & Appeals
Denial management is the process of comprehensively and systematically investigating every denial and understanding the root causes of why the claims were denied. Denial management involves analyzing common denial trends to redesign and improve the claim process to prevent future denials. Once a trend between the common denial reason codes and individual payer codes is established, the denial management team will correct these trends to improve on future claiming processes to reduce claim denials.
Appeals refer to the follow-up action once a submitted claim has been rejected by the payer, which is usually an appeal and improvement in mitigating potential denials. Appeals involve the preparation and submission of supporting documents about the claim such as medical records.
Denials are a substantial cost of the billing process and put a heavy strain on the healthcare providers’ resources and time. Denials represent persistent pain points and headaches for healthcare providers as a rough estimation of the cost of reworking a denied claim is roughly $25 per denial.
Each healthcare provider in the United States also spends roughly $5 million annually on claim denials, with most hospitals and healthcare providers experiencing an increase in claim denials over the past few years. Denied claims, therefore, represent lost or delayed revenue and would affect the healthcare provider’s cash flow especially considering the number of claims providers submit.
Key Features of Denial Management & Appeals
The denial management process involves uncovering and resolving the problems leading to the claim denial and shortening the accounts receivable cycle. If the healthcare provider has sufficient explanation and documentation for the claim, they can proceed to appeal if there is a reasonable expectation that the denied claim will be overturned.
The appeals process vary for different healthcare providers, but some of the key features are:
- Resending any failed appeals to include all required information and documentation
- Obtaining and completing all required forms
- Sending an appeal letter to address an incorrect name, personal information, invalid code, or modifier
- Collecting relevant or corrected patient information and documentation
- Calling the insurer to clarify confusion regarding denial codes
- Recording and obtaining reference numbers when contacting the insurer
Why Choose KR Billing Solutions?
KR Billing Solutions can identify the root causes of denials to increase your clean-claims rate. We can streamline the workflows and billing process to ensure faster appeals, improved cash flow, and greater efficiency. We are also HIPAA compliant and do all of our business onshore, whilst staying updated on local and national regulations and policies to reduce regulatory risk. You can rely on our expertise and team of seasoned professionals for your revenue cycle chain and billing process.
If you have any questions about denial management and appeals, you can call us at (855) 978-6499 or send us an email.
Need Our Help?
Prefer speaking with a human to filling out a form? call corporate office and we will connect you with a team member.
Denial Management & Appeals
KR Billing Solutions can handle all your billing needs and help you manage your revenue cycles to maximize your revenue and ensure constant cash flow. We have the capacity, software, and team members to handle the high volume of claims and denials and can address any lost revenue during our audits and tracking services.
About Denial Management & Appeals
Denial management is the process of comprehensively and systematically investigating every denial and understanding the root causes of why the claims were denied. Denial management involves analyzing common denial trends to redesign and improve the claim process to prevent future denials. Once a trend between the common denial reason codes and individual payer codes is established, the denial management team will correct these trends to improve on future claiming processes to reduce claim denials.
Appeals refer to the follow-up action once a submitted claim has been rejected by the payer, which is usually an appeal and improvement in mitigating potential denials. Appeals involve the preparation and submission of supporting documents about the claim such as medical records.
Denials are a substantial cost of the billing process and put a heavy strain on the healthcare providers’ resources and time. Denials represent persistent pain points and headaches for healthcare providers as a rough estimation of the cost of reworking a denied claim is roughly $25 per denial.
Each healthcare provider in the United States also spends roughly $5 million annually on claim denials, with most hospitals and healthcare providers experiencing an increase in claim denials over the past few years. Denied claims, therefore, represent lost or delayed revenue and would affect the healthcare provider’s cash flow especially considering the number of claims providers submit.
Key Features of Denial Management & Appeals
The denial management process involves uncovering and resolving the problems leading to the claim denial and shortening the accounts receivable cycle. If the healthcare provider has sufficient explanation and documentation for the claim, they can proceed to appeal if there is a reasonable expectation that the denied claim will be overturned.
The appeals process vary for different healthcare providers, but some of the key features are:
- Resending any failed appeals to include all required information and documentation
- Obtaining and completing all required forms
- Sending an appeal letter to address an incorrect name, personal information, invalid code, or modifier
- Collecting relevant or corrected patient information and documentation
- Calling the insurer to clarify confusion regarding denial codes
- Recording and obtaining reference numbers when contacting the insurer
Why Choose KR Billing Solutions?
KR Billing Solutions can identify the root causes of denials to increase your clean-claims rate. We can streamline the workflows and billing process to ensure faster appeals, improved cash flow, and greater efficiency. We are also HIPAA compliant and do all of our business onshore, whilst staying updated on local and national regulations and policies to reduce regulatory risk. You can rely on our expertise and team of seasoned professionals for your revenue cycle chain and billing process.
If you have any questions about denial management and appeals, you can call us at (855) 978-6499 or send us an email.
Need Our Help?
Prefer speaking with a human to filling out a form? call corporate office and we will connect you with a team member.
