- Home
- Credentialing Solutions
- Medicare Credentialing
Medicare Credentialing
Medicare Credentialing
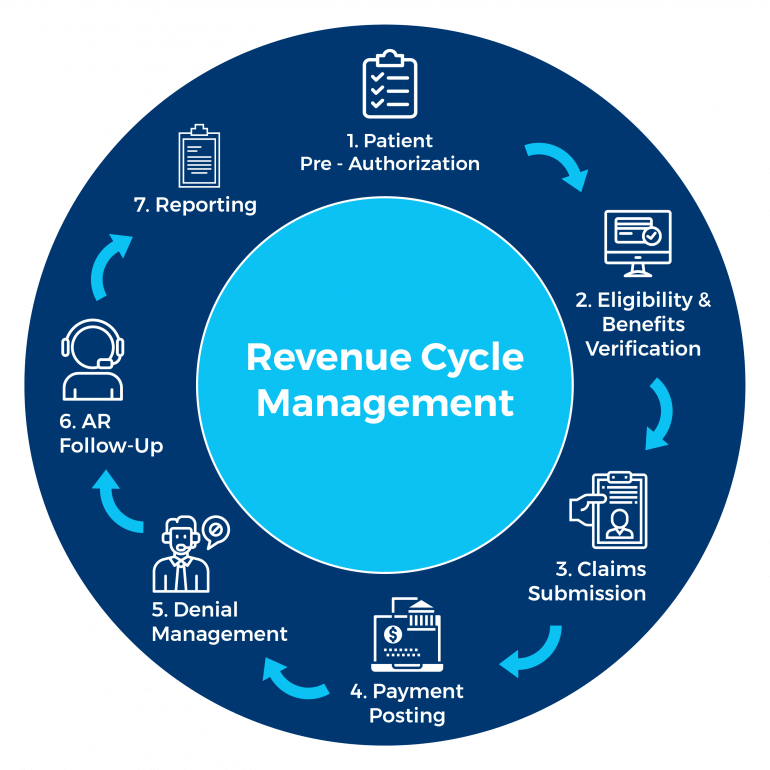
KR Billing Solutions provide billing solutions services for hospitals and clinics. We provide revenue management and help medical firms and hospitals to maximize their revenue by taking charge of the billing processes and ensure that claims are sent with accuracy and compliance. We also provide client support and will come up with a targeted and specific plan to suit your business needs.
About Medicare Credentialing
Medicare credentialing is a process of approving an agency, physician, or other medical providers as part of the Medicare supply chain. Medicare is the United States health insurance program that is administered by the Centers for Medicare and Medicaid Services.
Medicare providers thus serve Medicare beneficiaries and are paid for their services by Medicare rather than the individuals. Medicare credentialing may vary depending on the type of services the clinic or hospital provides. Medicare credentialing requires you to meet certain licensing and credentialing requirements to ensure that you possess the necessary qualifications for providing healthcare.
Medicare credentialing would require you to submit paperwork and documents such as practitioner licenses, diplomas, tax records, board certifications, proof of identification, and federal and state CDS certificates just to name a few. Do note that Medicare credentialing also has to follow state and federal requirements for your profession.
Why Is Medicare Credentialing Important?
Medicare credentialing is a process of approving an agency, physician, or other medical providers as part of the Medicare supply chain. Medicare is the United States health insurance program that is administered by the Centers for Medicare and Medicaid Services. Medicare providers thus serve Medicare beneficiaries and are paid for their services by Medicare rather than the individuals. Medicare credentialing may vary depending on the type of services the clinic or hospital provides.
Medicare credentialing is important as it requires you to meet certain licensing and credentialing requirements to ensure that you possess the necessary qualifications for providing health care. Medicare credentialing would require you to submit paperwork and documents such as practitioner licenses, diplomas, tax records, board certifications, proof of identification, and federal and state CDS certificates just to name a few. Do note that Medicare credentialing also has to follow state and federal requirements for your profession.
Who Needs Medicare Credentialing Services?
Medicare credentialing services are needed by healthcare companies, clinics, doctors, and physicians. This is because Medicare credentialing establishes your professionalism in a healthcare setting through documentation and verification by Medicare, and ensures that your practice is in line with federal and state laws.
Medicare credentialing services also help to protect healthcare organizations from revenue loss as they can claim reimbursement from Medicare.
Why Choose KR Billing Solutions for Medicare Credentialing?
KR Billing Solutions can help your company with Medicare credentialing. We can ensure a smooth and efficient application process through the Medicare Administrative Contractor so that you can focus on taking care of your patients and running your clinic or hospital. KR Billing Solutions is proud to have qualified and experienced professionals who can handle your billing needs and Medicare credentialing.
If you have any questions about Medicare credentialing, you can call us at (855) 978-6499 or send us an email.
Need Our Help?
Prefer speaking with a human to filling out a form? call corporate office and we will connect you with a team member.
