- Home
- Credentialing Solutions
- Medicaid Credentialing
Medicaid Credentialing
Medicaid Credentialing
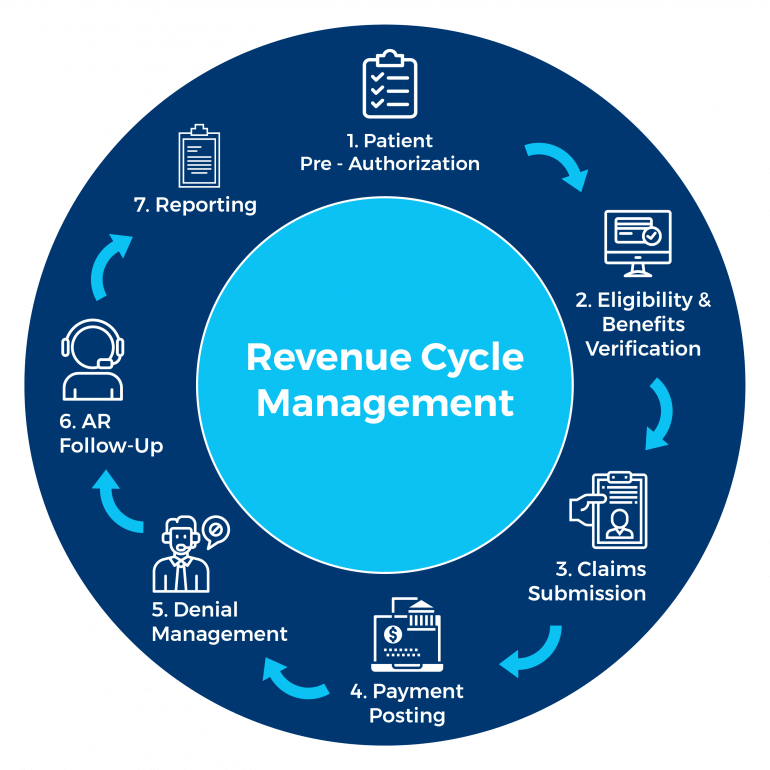
KR Billing Solutions is a leading provider of revenue cycle management solutions. We can help maximize your revenue practices, handle your billing needs, and account for all your revenue during transactions. We are always HIPAA compliant and we believe in adding a personal touch to the work that we do, which is why we do not automate or outsource our work.
About Medicaid Credentialing
Medicaid credentialing is needed for obtaining a Medicaid provider identification number. This identification number can be used by clinics, physicians, agencies, and healthcare providers to submit claims for healthcare services and receive reimbursement from the Medicaid program.
Medicaid credentialing thus refers to the process of approving healthcare providers, agencies, clinics, and physicians for the Medicaid program. Medicaid is a state and federal program in the United States which helps with the healthcare costs for low-income families and individuals. Medicaid also offers benefits that are not covered by Medicare, such as personal care services and nursing home services.
Why Is Medicaid Credentialing Important?
Medicaid credentialing is important because it ensures the quality of healthcare providers and agencies and professionals by Medicaid. It also improves patients’ trust in their healthcare providers and doctors as they know the qualifications of their doctors and healthcare providers. Medicaid credentialing is also important for healthcare providers and professionals as it ensures that they do not lose revenues and their medical services are reimbursed by insurance agencies.
Medicaid credentialing also lowers the risk of medical errors caused by incompetent healthcare providers. This supports the safety and security of the American healthcare industry. Credentialing also ensures that healthcare providers, agencies, and professionals have the necessary experience, facilities, and equipment to provide the highest level of care possible to their patients.
Who Needs Medicaid Credentialing Services?
Healthcare agencies, providers, and professionals should obtain Medicaid credentialing services as it is recommended for them to continue their practice and business. Medicaid credentialing is also necessary for maintaining high standards of safety in the medical profession as it verifies that the healthcare professionals are properly trained and certified.
Medicaid credentialing also allows healthcare providers, professionals, and agencies to participate in a healthcare network or treat patients at a hospital or medical facility. Medicaid credentialing allows you and your business to partner with insurance carriers such as Medicare and Medicaid. You are therefore able to obtain reimbursement for the medical services you provide.
Why Choose KR Billing Solutions?
KR Billing solutions will work daily to ensure your claims and appeals are submitted promptly and on time. We will also check to ensure that your claims are error-free and consistent. KR Billing solutions will ensure that your Medicaid credentialing process is efficient and hassle-free.
We understand the amount of detail and information needed for the Medicaid credentialing process and are committed to ensuring your business becomes credentialed as soon as possible.
If you have any questions about Medicaid credentialing, you can call us at (855) 978-6499 or send us an email.
Need Our Help?
Prefer speaking with a human to filling out a form? call corporate office and we will connect you with a team member.
